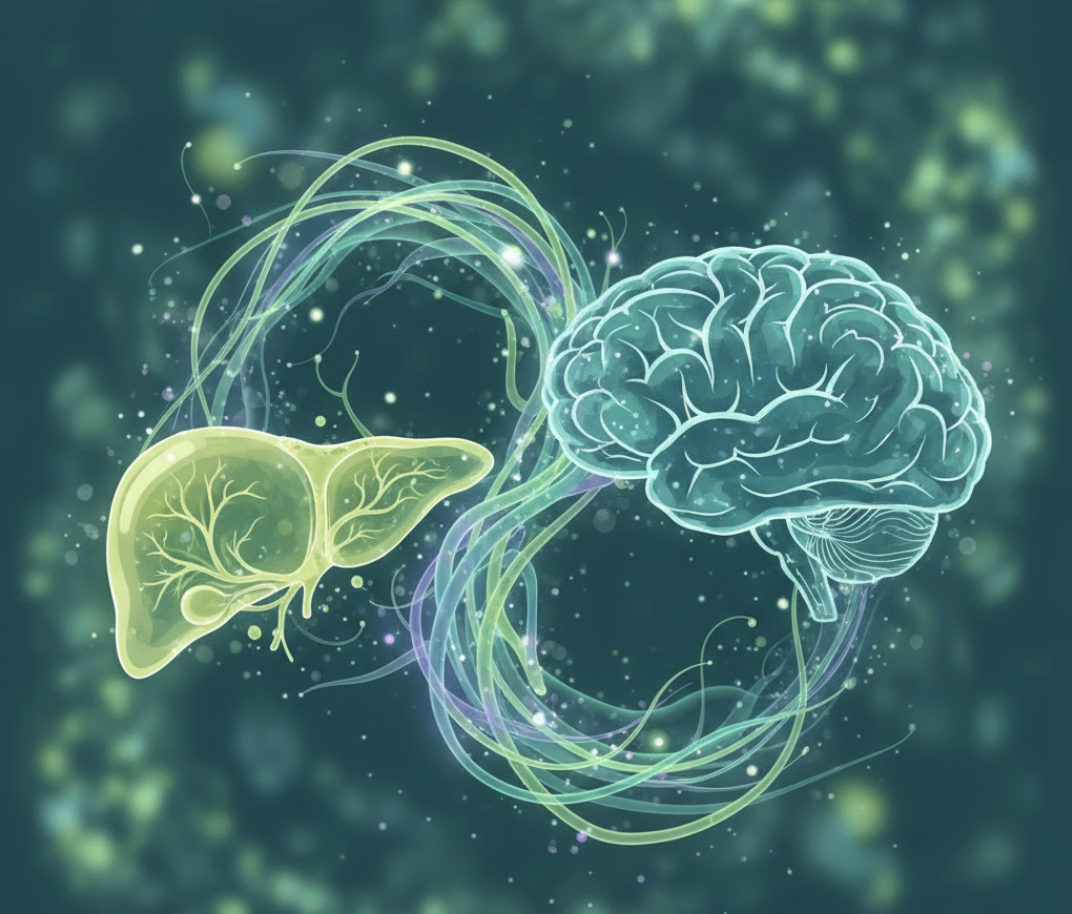
When you think about liver disease, you might picture pain, fatigue, or digestive problems. But there’s another side: Mental Health. Depression, anxiety, stress, and even cognitive changes often travel hand-in-hand with liver conditions. And understanding this link is essential if we want to treat patients fully and early.
What We Know About This Link?
A recent meta-analysis of over 2 million adults with non-alcoholic fatty liver disease (NAFLD) found that roughly 26% had depression, 37% had anxiety, and 51% experienced stress. Those are high numbers. Essentially, more than one in four people with NAFLD are also dealing with mood issues.
Another study using Mendelian randomization found that genetic predisposition to fatty liver disease raises the risk of psychiatric disorders, including bipolar disorder, post-traumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD). This suggests that it’s not just lifestyle or external stressors that could be biological drivers linking liver pathology and mental health.
Meanwhile, in people with chronic liver disease (CLD), mood disorders don’t just reduce quality of life; they worsen clinical outcomes. A review in Hepatology Communications showed that patients with depression and anxiety often have worse symptoms, lower adherence to treatment, greater fatigue, impaired social participation, and increased mortality risk.
The Vicious Cycle
The relationship is bidirectional. Not only does liver disease increase the risk of mental health disorders, but untreated mental health problems can worsen liver disease outcomes. For example:
-
Depression and anxiety significantly decrease adherence to treatment plans and healthy behaviors, accelerating disease progression.
-
Poor mental health increases the likelihood of substance use, which can further damage liver function.
-
Fatigue, pain, and impaired sleep from either liver disease or comorbid mental illness can amplify one another, lowering quality of life and complicating diagnosis and care.
Why Early Detection & Integrated Care Matter
Recognizing mental health symptoms early in liver disease can change the trajectory:
-
Improved treatment adherence: Someone who isn’t depressed or deeply anxious is more likely to follow dietary, lifestyle, or medication recommendations.
-
Better quality of life: Managing anxiety, depression, or stress helps patients maintain social connections, continue daily activities, work, and sleep, all of which support physical health.
-
Reduced progression risk: Early lifestyle interventions or medical monitoring can slow disease progression. If mental health improves, energy and motivation to act improve.
How Tools Like LIVERFASt™ & LIVERSTAT Fit?
At Fibronostics, we believe in holistic care. While mental health may lie outside the “traditional” scope of liver diagnostics, non-invasive tools like LIVERFASt™ and LIVERSTAT are essential ingredients in a full picture because:
-
By detecting fibrosis, steatosis, and inflammation early, they allow clinicians to intervene before physical disease becomes severe (and before symptoms like fatigue, brain fog, and mood changes become overwhelming).
-
For individuals experiencing anxiety or mild mood issues, knowing one’s liver health status can reduce uncertainty and fear. Often, fear and “not knowing” contribute heavily to mental distress.
-
They provide measurable, repeatable data, which helps guide both medical and lifestyle interventions, knowing where you stand and seeing progress supports motivation and mental well-being.
Conclusion
The intricate connection between the liver and mental health emphasizes that optimal care for individuals with liver disease must address both physical and psychological needs. Mental health symptoms are not just a byproduct of chronic disease; they are closely tied to the underlying biology of liver dysfunction. Integrated care, early intervention, and mindful attention to both mind and body are crucial for improving overall quality of life and clinical outcomes in this vulnerable population